INTRODUCTION
Patients suffering from acute myocardial infarction with ST-segment elevation (STEMI) have a high hospital mortality rate, which, according to various records, ranges from 7% to 9%, (1,2,3), is higher in patients with heart failure (HF) at admission, (4) and depends on the treatment received. (5,6,7)
Since the 1967 work by Thomas Killip and John Kimball (KK), who described the clinical characteristics of patients with STEMI, prognosis has improved thanks to coronary reperfusion strategies. As a result, the percentage of patients classified as Killip and Kimball class A (KK A) has increased dramatically from 33% to 78%, making it the most common clinical presentation at hospital admission in patients with STEMI. However, few studies have analyzed complications or hospital mortality specifically in this patient subgroup.
In the era of reperfusion therapy, a decrease in complications in patients with STEMI has been observed, enabling earlier hospital discharge. (10,11) In countries such as the United States, the average length of hospitalization is three days, International guidelines recommend early discharge (on the third day) in low-risk patients, with conditions such as age
<70, left ventricular ejection fraction (LVEF) >45%, 1- or 2-vessel disease, successful coronary angioplasty, and absence of arrhythmias. (12) Despite this, early discharge is not always implemented, even in eligible patients.
Objectives:
To determine the incidence of the KK class A at admission in patients with STEMI and its role in overall mortality.
To establish the incidence of HF during the clinical course of patients classified as KK A at admission and its characterization. To analyze the negative predictive value of the absence of HF during the clinical course on mortality.
METHODS
This study was conducted as a retrospective analysis of the ARGEN-IAM-ST continuous registry, a prospective and observational registry of hospitalized STEMI patients. The study was performed from March 2015 to October 2024, and its design focused on assessing the hospital clinical course of patients with KK A admitted to the coronary care unit.
The inclusion criteria were patients classified as Killip and Kimball classes A, B, C, or D, according to the original Killip and Kimball classification. A total of 264 patients were excluded: 174 due to missing data, and 90 because of mechanical complications. HF was classified as a hospital complication. The diagnosis of HF was based on the treating physician’s criteria according to the Killip and Kimball classification. Bleeding was defined as follows: minimal: nonintracranial, with a decrease in hemoglobin (Hb) <3 mg/ dL; minor: non-intracranial with a decrease in Hb between 3 and 5 mg/dL; major: intracranial bleeding or a decrease in Hb >5 mg/dL.
Statistical analysis
Quantitative variables with normal distribution were expressed as mean and standard deviation (SD), while those with non-normal distribution were reported as median and interquartile range (IQR). To perform the statistical analysis of these variables, the Student's t-test, Mann-Whitney U test, or analysis of variance (ANOVA) were used as appropriate.
Qualitative variables were expressed as frequencies and percentages, and the statistical analysis was performed using the chi-square test or Fisher's exact test, as appropriate. A contingency table was created to explore an association between the presence or absence of HF and the clinical
course in patients with KK A at admission.
The search for independent predictors of progressive HF and the assessment of the incidence of progressive HF on the occurrence of events were conducted using multiple logistic regression analysis, including variables that were statistically significant in the univariate analysis. The association with events was expressed as odds ratio (OR) with its 95% confidence interval (95% CI). A p value <0.05 was considered statistically significant. To assess the usefulness of the overall model (Table 2), the omnibus test was used, and a ROC curve was generated. The statistical analysis was performed using the statistical software JAMOVI (version 2.3.28.0).
Table 1
Baseline characteristics of patients according Killip and Kimball classification at admission
| Variable | KK A (n=5666) | KK B (n=1020) | KK C (n=107) | KK D (n=511) | p |
|---|---|---|---|---|---|
| Age, years | 60 (52-68) | 63 (55-72) | 64 (56-74) | 64 (57-74) | <0.001 |
| Female sex | 20 | 23 | 29 | 29 | <0.001 |
| Diabetes mellitus | 26 | 31 | 34 | 34 | <0.001 |
| Hypertension | 52 | 58 | 66 | 65 | <0.001 |
| Dyslipidemia | 37 | 38 | 43 | 36 | 0.601 |
| Smoking | 31 | 34 | 35 | 35 | 0.061 |
| Prior AMI | 37 | 54 | 59 | 39 | <0.001 |
| Symptom-to-door time, min | 119 (55-240) | 129 (60-300) | 152 (60-323) | 120 (53-300) | 0.004 |
| Reperfusion therapy | 91 | 88 | 84 | 87 | <0.001 |
| Ischemic total time (PCI), min | 305 (185-573) | 345 (198-660) | 524 (271-901) | 400 (212-722) | <0.001 |
| Ischemic total time (FBL), min | 180 (105-290) | 220 (120-327) | 170 (112-266) | 180 (104-329) | 0.399 |
| Reperfusion therapy: | 80 | 74 | 77 | <0.001 | |
| Primary PCI | 13 | 76 | 16 | 11 | |
| Fibrinolytics | 7 | 13 | 9 | 12 | |
| Both | 11 | ||||
| Door-to-balloon time, min | 77 (44-135) | 80 (43-130) | 102 (60-198) | 85 (50-141) | 0.004 |
| Multivessel disease | 32 | 41 | 46 | 52 | <0.001 |
| Successful PCI | 98 | 95 | 90 | 84 | <0.001 |
| Bleeding: | <0.001 | ||||
| Minimal | 2 | 3 | 7.5 | 6 | |
| Minor | 0.7 | 0.9 | 5 | 3 | |
| Major | 0.5 | 0.8 | 0.9 | 1.4 |
AMI: acute myocardial infarction; FBL: fibrinolytics; KK: Killip and Kimball; PCI: percutaneous coronary intervention.
Qualitative variables are expressed as percentage rounded to the nearest whole number. Quantitative variables are expressed as median and interquartile range.
Ethical considerations
The protocol was reviewed and approved by the Bioethics Committee of the Argentine Society of Cardiology. This registry does not require signed informed consent. This decision is left to each participating institution.
RESULTS
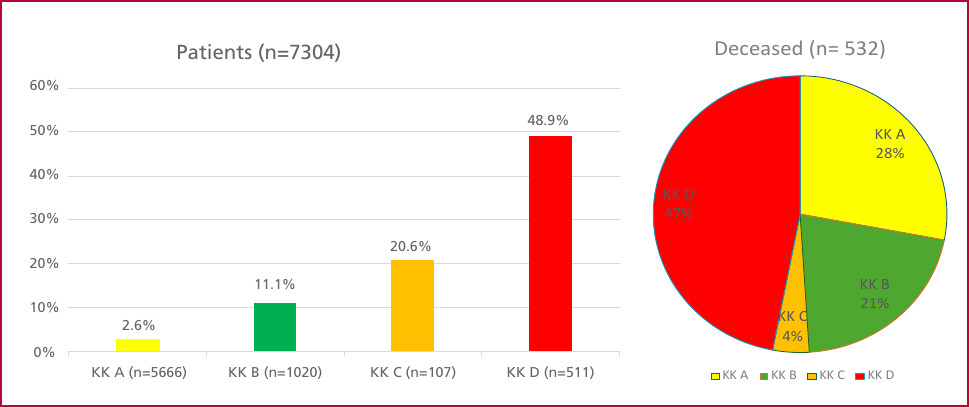
From March 2015 to October 2024, 7304 patients were admitted for STEMI, with a median age of 60 years (IQR 52-67), 80% were male. According to Killip and Kimball classification, 77.6% of patients were class A (n=5666), 14% class B (n=1020), 1.4% class C (n=107), and 7% class D (n=511).
Table 1 shows the baseline characteristics of patients according to KK classification at admission. KK A patients were significantly younger, less likely to be female, had lower prevalence of diabetes, hypertension, prior acute myocardial infarction (AMI) location, and shorter symptom-to-door time. They also had a lower prevalence of multivessel disease but a higher use of primary percutaneous coronary intervention (PCI) as their revascularization method. The rate of successful primary PCI was higher in this group.
Among KK A patients, 311 (5.4%) developed progressive HF during hospitalization. Their baseline characteristics resembled those of patients with KK class >A (Table 2). In a multiple logistic regression model, the independent variables associated with progressive HF were age >70 years, female sex, diabetes, anterior descending artery involvement, symptomto-door time, and failed primary PCI (area under the ROC curve 0.68, 95% CI 0,61-0,74) (Table 3).
Table 2
Baseline characteristics of Killip and Kimball class A patients according to the presence or absence of progressive heart failure
| Variable | HF (n=311) | Non-HF (n=5355) | p |
|---|---|---|---|
| Age, years | 64 (56-74) | 60 (52-67) | <0.001 |
| Female sex | 28 | 19 | < 0.001 |
| Diabetes mellitus | 32 | 25 | <0.001 |
| Hypertension | 59 | 52 | 0.001 |
| Dyslipidemia | 41 | 37 | 0.101 |
| Smoking | 31 | 34 | 0.551 |
| Prior AMI | 47 | 36 | <0.001 |
| Symptom-to-door time, min | 120 (60-300) | 116 (55-240) | <0.001 |
| Reperfusion therapy | 91 | 91 | 0.991 |
| Ischemic total time (PCI), min | 377 (203-818) | 300 (183-568) | <0.001 |
| Ischemic total time (FBL), min | 200 (110-324) | 180 (105-285) | 0.512 |
| Reperfusion therapy: Primary PCI Fibrinolytics Both | 75 17 8 | 81 12 7 | 0.033 |
| Door-to-balloon time, min | 83 (48-150) | 77 (44-135) | 0.255 |
| Culprit vessel: LADA | 60 | 43 | <0.001 |
| Successful PCI | 91 | 98 | < 0.001 |
| Bleeding Minimal Minor Major | 4 3 2 | 2 0.5 0.4 | <0.001 |
AMI: acute myocardial infarction; FBL: fibrinolytics; HF: heart failure; LADA: left anterior descending artery;min: minutes; PCI: percutaneous coronary intervention.
Qualitative variables are expressed as percentage rounded to the nearest whole number. Quantitative variables are expressed as median and interquartile range.
Table 3
Multivariate analysis of the development of progressive heart failure
| Variable | OR | 95% CI | p |
|---|---|---|---|
| Age >70 | 2.06 | 1.51-2.81 | <0.001 |
| Female sex | 1.65 | 1.20-2.26 | 0.001 |
| Diabetes mellitus | 1.71 | 1.27-2.31 | <0.001 |
| Culprit vessel: LADA | 1.88 | 1.26-2.81 | 0.001 |
| Symptom-to-door time, min | 1.04 | 1.03-1.06 | 0.022 |
| Failed PCI | 4.20 | 2.42-7.28 | <0.001 |
HF: heart failure; LADA: left anterior descending artery; PCI: percutaneous coronary intervention; OR: odds ratio
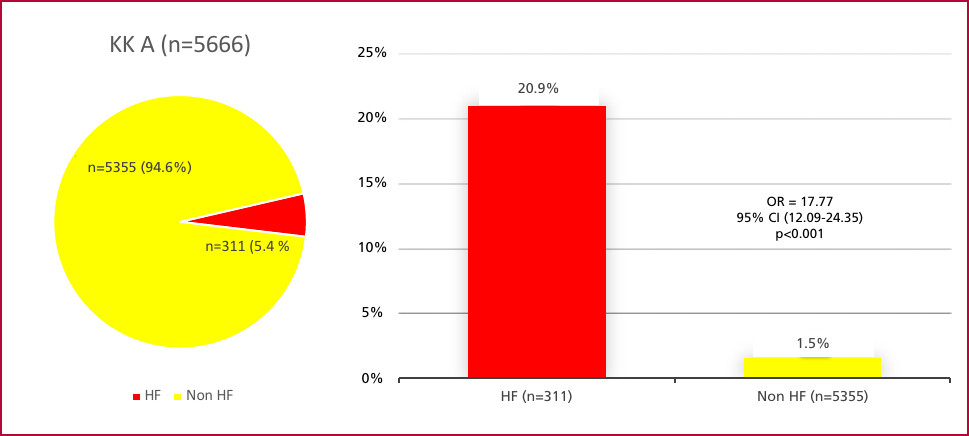
Total in-hospital mortality was 7.3% (n=532). Among patients with KK A, in-hospital mortality was 2.6%, accounting for 28% of total deaths (Figure 1). Among the 311 KK A patients who developed progressive HF, in-hospital mortality was 20,9% (n=65), while it was only 1.5% (n=82) among the 5355 patients who did not (OR 17.77, 95% CI 12.09-24.35; p<0.001). In the multivariate analysis in KK A patients, the development of HF was an independent predictor of hospital mortality (OR 4.79; 95% CI 2.74-8.36 p<0.001).
Fig. 1
Mortality rate according to Killip and Kimball classification at admission (bar chart). Percentage impact of deaths according to Killip and Kimball classification on overall mortality for myocardial infarction (pie chart).
DISCUSSION
The Killip and Kimball (KK) classification, proposed in 1967, (8) continues to be a valid and widely used tool for risk stratification in STEMI patients. Despite the time elapsed and therapeutic advances, its simplicity, reproducibility, and prognostic value have preserved
its clinical utility. However, the patient profile has changed considerably since its original publication. (9) In particular, there is now a higher proportion of patients admitted to KK class A, a phenomenon attributable to the positive impact of adjuvant therapies, especially early reperfusion treatment. (13,14)
In our study, we observed that the vast majority of STEMI patients were admitted to KK class A. This subcategory, despite its low individual mortality, represents a significant proportion of AMI-related deaths: approximately one in three occurs in this group. This finding, in line with our first objective, highlights that initial classification in KK class A does not guarantee an event-free hospital course. In fact, the high prevalence of this subcategory has a significant impact on overall AMI mortality, a fact that, although little explored in previous studies, is essential for an adequate understanding of population risk.
Likewise, in addressing our second objective, we identified that approximately 5% of patients admitted to KK class A developed HF during hospitalization. Among them, 21% died before discharge, underscoring the adverse prognostic impact of HF as a hospital complication. (15) The progression to HF in this subgroup, initially considered low risk, highlights the need for continuous clinical monitoring and more sensitive risk stratification strategies. (16,17) In this regard, multivariate analysis allowed us to identify independent predictors for the development of HF, which are similar to those in the PAMI II study and the Zwolle score. (18,19,20,21,22,23) However, the model discriminatory power was moderate, with a C-statistic of 0.68, indicating the need to optimize predictive tools for this population.
On the other hand, patients who did not develop HF during hospitalization had a very favorable outcome, with a low event rate, which translates into a high negative predictive value. This observation supports the consideration of this subgroup for early discharge strategies, (24,25,26,27,28) in line with international guidelines (Class IIa recommendation). (29,30) Additionally, clinical detection of HF may be complemented by B-type natriuretic peptide (BNP) testing,(31) which has proven useful for early identification of ventricular dysfunction even in the absence of overt clinical signs, as shown by the GREAD NETWORK registry. (32)
Multiple studies have confirmed that HF at admission is associated with a worse prognosis in the context of acute coronary syndrome. (4,15) However, our study offers a different perspective, shifting the focus to HF as a progressive event in patients classified as KK A at admission. This view contrasts with previous studies from the ARGEN-IAM-ST registry, which focused exclusively on patients with KK class B, C, or D at admission, (33,34,35,36) leaving a gap in understanding the clinical course of those initially considered low risk.
Finally, our findings allow us to assess the epidemiological burden of KK A patients on overall STEMI mortality and highlight that HF onset during hospitalization is a critical event with significant prognostic implications. Conversely, the absence of HF is asso-
ciated with a favorable outcome, which has important clinical implications for decision-making regarding early discharge and outpatient follow-up. This information emphasizes the importance of a dynamic approach to risk stratification that considers both the initial clinical presentation and the hospital clinical course.
Limitations
Due to the design of the ARGEN-IAM-ST registry, we were unable to determine the exact timing of HF onset. However, we can estimate this indirectly, as most complications in our local clinical context occur within
CONCLUSIONS
KK A at admission remains a valid criterion for identifying patients who will have a favorable hospital course following STEMI. However, close monitoring in the coronary care unit is essential to detect patients who will develop heart failure, as they constitute a high-risk group for early discharge.
Conflicts of interest
None declared.
(See authors' conflict of interests forms on the web).