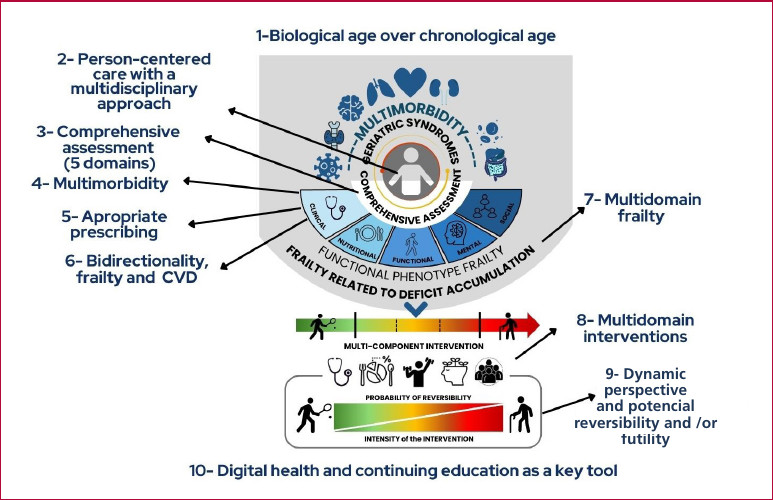
In March of this year, the first position paper on frailty and comprehensive assessment in cardiology was published (1), developed during 2024 and presented at the 50th Argentine Congress of Cardiology. During a recent council meeting attended by leaders from across Ibero-America, the spirit of the document was summarized in ten key points. The objective of this decalogue is the dissemination of these key concepts and their incorporation into daily clinical practice.
1. Emphasize biological age over chronological age and eliminate the term "special population": While we recognize the influence of chronological age, the ageist concept is only a biased and partial viewpoint in decision-making due to the significant heterogeneity within the population. The impact of multimorbidity, polypharmacy, socioeconomic conditions, among other factors, and the different models of vascular aging mark the discordance between them. In turn, the term "special populations," coined years ago to refer to older people, is obsolete and imprecise, as this is usually the most significant population group in the epidemiology of cardiovascular diseases. (1,2)
2. Prioritize person-centered care with a multidisciplinary approach: We prioritize the individual over the disease in decision-making and acknowledge the role of the social environment and a multidisciplinary team in patient care. (1,3)
3. Conduct a comprehensive assessment based on five domains: We incorporate nutrition into the classic domains of geriatrics (clinical, functional, mental, and social) due to its impact on different cardiovascular diseases and vice versa. A comprehensive assessment allows us to identify specific vulnerabilities and guide personalized interventions, prioritizing those domains that affect prognosis and quality of life. (1)
4. Emphasize the concept of multimorbidity over comorbidity: Multimorbidity, an expanded concept of comorbidity, stands out as a geriatric syndrome in geriatric cardiology due to its high association with adverse cardiovascular events. It refers to the presence of several chronic diseases, clinical and non-clinical conditions in the same person, transversally, without dominance or interrelation of one over the other. (1,4)
5. Promote appropriate prescribing: In the field of cardiology, it is not uncommon to encounter patients who are taking multiple medications due to the high prevalence of multimorbidity. Polypharmacy, a global issue, refers to the use of five or more medications, irrespective of whether they are prescribed. It is imperative to distinguish between appropriate and inappropriate polypharmacy, and in the latter case, to promote deprescribing. As a response to this problem, our working group is developing a document on Appropriate Medication in Cardiovascular Therapy (MATE, acronym of the name in Spanish Medicación Adecuada en TErapéutica Cardiovascular). (1,3,5,6)
6. Acknowledge the bidirectional relationship between frailty and cardiovascular disease: Multiple reviews have evaluated and documented the relationship between frailty and adverse cardiovascular events. It has been demonstrated that both entities share risk factors and that there is a negative feedback between them. Consequently, intervention measures on either one have a direct impact on the other. (1,7)
7. Assessment of frailty in relation to deficit accumulation (multidomain): Our guideline supports a comprehensive assessment because, although frailty has an impact on functionality, it provides a partial view of the problem. However, we emphasize the role of the functional domain as one of the pillars of the comprehensive assessment and evaluation of frailty in relation to the accumulation of deficits. (1,7,8)
8. Promote multidomain interventions: Once the comprehensive assessment has been carried out, the interventions should target the different domains. We emphasize the significance of paying close attention to clinical conditions, polypharmacy, vaccinations, the adaptation of nutritional plans, multicomponent exercise, and psychosocial interventions. (1,4,6)
The acronym "VIDA" (Vaccination, drug Interaction, Diet, physical Activity) is the starting point for the design of a new position paper on prevention and tools for a better quality of life.
9. Dynamic perspective and potential reversibility and/or futility: We emphasize the need to address the concept of "frailty" from a dynamic perspective that considers different situations: pre-frailty, mild, moderate, and severe frailty. Each one offers potential interventions for reversibility, since early and timely detection can make a difference in quality of life.
It is imperative to identify and avoid futile interventions, incorporate palliative care and comfort when appropriate, promote person-centered medicine
through therapeutic adaptation based on patient values and preferences and their social and family environment, and implement preventive measures. All these principles constitute the pillars of person-centered medicine. (1,7,8)
10. Digital health and continuing education as key tools: New digital health technology tools must be applied and adapted for the assessment and treatment of older adults in order to provide care and quality of life.
Finally, none of the aforementioned changes will be possible unless geriatric cardiologists are included in the training of cardiologists and other related specialties. (1,9)
Central illustration
Decalogue of the position paper and comprehensive assessment in cardiology CVD: cardiovascular disease
Conflicts of interest
None declared.
(See conflicts of interest forms on the website).
Acknowledgments
The authors express their gratitude to the Clinical Practice Standards and Consensus Statements Area of the Argentine Society of Cardiology, and to Daniel Piñeiro (World Heart Federation), Robinson Cuadros (Latin American Committee of the International Association of Gerontology and Geriatrics), Pablo Stutzbach, Mario Spennato, and Jorge Trongé (Argentine Society of Cardiology), José Ángel Pérez Rivera (Spanish Society of Cardiology), Alberto Barón and Jerson Quitián (Colombian Society of Cardiology), Yalile Nahúm (Chilean Society of Cardiology), Alexandra Castillo (Dominican Society of Geriatrics), Amir Gómez León Mandujano (Mexican Society of Cardiology), Adriana López (Chilean Society of Geriatrics and Gerontology), and Matías Manzotti (Argentine Society of Gerontology and Geriatrics), for their valuable and selfless contributions.
